Get A Dental Insurance Quote
- COMPARE PLANS
-
VIEW QUOTES NOW!
In-Network vs Out-of-Network Dental Insurance Coverage
Dental Shop Staff Writer | August 29, 2019
What is an in-network dental provider?
An in-network dental provider is a provider who has accepted the insurance companies fee schedule and has agreed to have a discounted maximum allowable charge for covered services as long as the member uses a provider within the network. Choosing a dentist within a network will limit your options.
What is an out-of-network dental provider?
Out-of-network providers are not a part of an insurance company's network of dental providers.
What is the difference between a PPO, indemnity, and HMO plan?Indemnity plans do not have a network of dentists and will pay where ever you go. They tend to be more expensive than the other types of plans, but they offer the most flexibility in choosing dental care providers. A HMO plan will ONLY cover in-network dentists; these plans are more affordable but at the expense of flexibility and possibly the quality of services. HMO plans tend to be more rare. PPO plans will cover BOTH in-network and out-of-network dentists. With a PPO plan, it will be cheaper to visit an in-network dentist. If you go out of network, you will generally still receive some coverage, but typically you will get better coverage going to an in-network provider.
If I have a PPO plan and go out of network, how much will I have to pay?
The amount you would have to pay depends on the insurance company's policy on out-of-network charges. Some companies will just have you pay the difference in what the usual and customary charge is and what the dentist you went to see charges, plus the percentage you would have paid under the policy. The usual and customary cost is determined by what the typical cost for that particular service is in your area. View your plan's brochure to see how your specific plan covers in-network and out-of-network dentists.
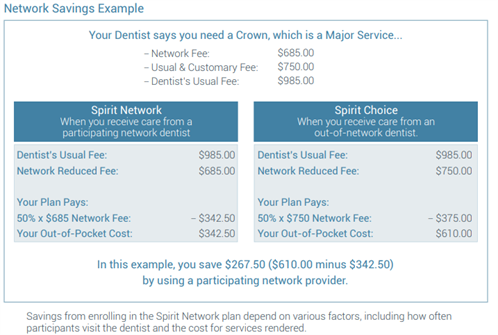
Below is an example of network savings in a Spirit Dental Plan
Tags:

